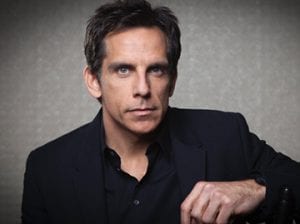
Ben Stiller, one of the few comedians on this side of the pond who can make me laugh, said that PSA testing saved his life. I suspect he wasn’t being funny. Mr Stiller had Gleason Grade 7 localized prostate cancer.
Is he right?
The honest answer is that we don’t know for certain. Before I get granular, we must visit proof, level of proof, and burden of proof. The statement “there’s no proof that Stiller’s life was saved by testing for PSA” is correct. But the statement can’t be made without determining on whom the burden of proof lies. Is it on those who say that PSA saved Stiller’s life, or on those who say that PSA did not save Stiller’s life?
We can’t ask for proof without stating what level of proof we’ll accept. Many won’t believe immaculate conception unless they witness it. You can disprove that Julius Caesar existed if the only proof you’ll accept is photographic evidence of his existence. In medicine, level of proof is a sliding scale which you can arbitrarily choose depending on what you wish disproven. Observational studies are no proof unless they prove what you want proven. RCTs are proof unless they disprove what you don’t want disproven.
It’s easy to confuse evidence for proof. To say there’s no proof that screening saved Stiller’s life is really saying there’s no evidence that screening has a net survival benefit. The key word is “net,” which, as you may recall from your tax returns, involves subtraction. If the “net” is zero, it doesn’t mean it was zero before the subtraction. Net benefit from screening can be zero if treating prostate cancer found by screening causes the same number of deaths as lives saved by screening.
What does “saving a life” in screening even mean? It should mean making a person live longer than they would have lived if they weren’t screened. This is difficult to capture. Statistically, “screening saves lives” means fewer deaths from the cancer that is being screened—in the case of PSA screening, fewer deaths from prostate cancer.
If PSA screening, hypothetically, saves Peter, Tom, and Rajeev but kills—because of complications of surgery—Dick and Anil, the net benefit is one. If it also kills Donald, the net benefit is zero. But here is the important point: Even if the net benefit of screening is zero, it still means that Peter, Tom, and Rajeev were saved by screening. I’m amazed that this elementary logic, which can be understood by most middle schoolers, eludes many doctors.
The statement “there’s no proof that Stiller’s life was not saved by PSA” is also correct. Some get nonjudgmental and say, “There’s no more proof that PSA saved Stiller’s life than a magical sky pixie saved Stiller’s life.” This cute, yet sophomoric, reasoning misses a point, which is that a PSA test leading to the discovery of a localized prostate cancer of intermediate grade could plausibly have saved Stiller’s life. What’s plausible is down to expertise and judgment, and such nonjudgmentalism that holds PSA testing in the same evidentiary bracket as a magical sky pixie, that is egalitarian with expertise, is not objective but idiotic.
It is, therefore, plausible and possible that PSA testing saved Stiller’s life, but is it probable? This is the crux of the disagreement and depends more on the prognosis of Stiller’s tumor than the net survival benefit of PSA screening. Let’s consider the latter. The net survival benefit of PSA screening is contentious. The Göteborg trial showed that screening for prostate cancer had a measurable treatment effect and that 293 people had to be invited for screening to prevent one death from prostate cancer. That’s impressive. For comparison, the number needed to screen to reduce death from lung cancer in heavy smokers is 320. The Prostate, Lung, Colorectal and Ovarian (PLCO) trial contaminated[2] because 90% in the control group had a PSA test. The PLCO trial compared PSA testing with PSA testing and found, unsurprisingly, that the group that received PSA testing didn’t live longer than than the group that received PSA testing.
What about the prognosis of Mr Stiller’s tumor? According to Dr Benjamin Davies, associate professor of urology at the University of Pittsburgh, Gleason 7 is precisely the tumor grade that benefits from early detection. It is neither so innocuous that treatment is redundant, nor is it so aggressive that treatment is forlorn—meaning, if left alone, it has a high chance of metastasizing and causing misery and early death. Ironically, Mr Stiller is the worst example for anti-PSA screening.
Screening is beyond net survival benefits. PSA screening can lead to harms from surgery or radiation therapy to the prostate. The value, or disutility, of a harm is subjective and personal. Whilst no man I know will ask Santa Claus for impotence for Christmas, some men would rather die standing than live hanging—meaning that for them, impotence is a fate worse than dying early from prostate cancer. Others might want to climb mountains rather than summit molehills—ie, they want to live as long as they can. There’s no “one size fits all” (pun unintentionally intended). Screening is the mother of all “one size fits all.” You might be your neighbor’s keeper, but you don’t own your neighbor’s values.
It gets even more complicated. Urologists are getting better at sparing nerves during prostate surgery. Thanks to advances in MRI, urologists are also getting better at identifying cancers that can safely be watched. Then there is the blue pill, which has softened prostatectomy’s most feared complication. The sledgehammer is getting more nuanced. Harms have reduced. Assessment of screening, which incorporates the harms of the past, not the present, is like basing US foreign policy today on the Cold War. This is why USPSTF has erred by excluding urologists, and other specialists, from its panel. Whilst urologists may not know more epidemiology than epidemiologists, they’re arguably more likely to pay attention to the strengths and weaknesses of the trials—it’s their livelihood. It’s a bias for sure, but a bias in the direction of the truth. The war against expertise is the strangest battle in a country that covets expertise.
The only objection to screening is philosophical—ie, what you view the role of medicine in society to be. FWIW, I wouldn’t support screening were I the healthcare czar. But I won’t pretend that my objections are empirical, because it is impossible to make a rational empirical objection to any one screening test without specifying, ex ante, the precise treatment benefit and its uncertainty needed before approval. The harms, as I alluded to, are subjective and a moving target. It is inconsistent to hold screening for prostate cancer to all-cause mortality reduction (highest standard of proof), yet to approve screening for colorectal cancer, which has not met that bar.[3]
I understand why urologists are pissed off that USPSTF has knocked down PSA testing but not mammograms. On its face, and even exploring more deeply, there seems to be little justification. The prostate, an organ which doesn’t have the prettiest real estate—separated, though it is, from the rectum by the tough fascia of Denonvillier—is a neglected child. But someone must look after it. And it’s disheartening that whilst us boys wear pink to increase breast cancer awareness, the sisters never return the favor. When was the last time you saw a woman wearing blue to increase prostate cancer awareness?
Screening, an individual choice, has become a societal prerogative. This is bound to cause cognitive dissonance. Some have adopted a middle ground and said that screening should be down to shared decision-making. How will you conduct shared decision-making for PSA screening? It’s not as easy as you think. Let me present a vignette.
Rajeev: “My wife wants me to get my PSA tested.”
Doctor: “Hold on, Rajeev. Let’s first engage in shared decision-making. I’m going to give you possibilities about your future and then explore your values, culture, and expectations before integrating them with the best available evidence so that you can make an informed decision about whether to pursue a PSA test.”
Rajeev: “You…what?”
Doctor: “Here is your future:
1. You will dies from a urinary tract infection in a nursing home, abandoned by your family and friends.
2. You will die an early and miserable death from prostate cancer if not screened and will also miss your daughter’s wedding.
3. If screened and a cancer is found and treated, you will live much longer and celebrate more birthdays.
4. If screened and a cancer is found and treated, you will die at the same time as you would have if you weren’t screened.
5. If screened and a cancer is found and treated, you will be left impotent and still die from a urinary tract infection in a nursing home, abandoned by your family and friends.
6. You and I will both be blown up by ISIS or have to build a wall along the 28th parallel.”
Rajeev: “You’re confusing me, doctor. Which one of these will happen to me?”
Doctor: “Your guess is as good as mine.”
Sure, throw some numbers to help Rajeev make an informed choice. But I suspect that Rajeev, and others from his culture, won’t care too much about probabilities. You’re the doctor, not he. He has come to you for your opinion, not his.
Which gets me back to Stiller. Some say he’s spreading misinformation by advocating PSA screening. I’d argue that it’s not possible to spread misinformation about screening because we don’t have a clue. Screening is an information problem; some benefit, some are harmed, but we don’t know who will benefit or who will be harmed. This has a name. It’s called “uncertainty.” I’m a huge advocate of public uncertainty. The more uncertain the public is, the less vice-like grip certitude has over them, the less religious and dogmatic they are, the better the world will be.
Ben Stiller has increased the public uncertainty about PSA screening. I think that’s a good thing.
From Medscape Radiology, republished by thehealthcareblog.com